Menopause in CF
With the increase in age of survival in CF, menopause is becoming a health experience that women with CF are now facing. Although there is limited research in this area in the CF population, it is known that women with CF are most likely to experience menopause 2-3 years earlier than those women without CF. The average age for a woman to experience menopause is between the ages of 49-51.
Menopause is defined as a time in a woman’s life 12 months after their last period. If during that 12-month time, there has been any spotting or occasional bleeds then the 12 months resets until the woman has had 12 months with no bleeding.
Perimenopause is the time in a woman’s life prior to reaching menopause, this can be up to 5-10 year prior to menopause. Changes in hormone levels are constantly occurring during this time, and there can be significant fluctuations in levels, with no specific pattern.
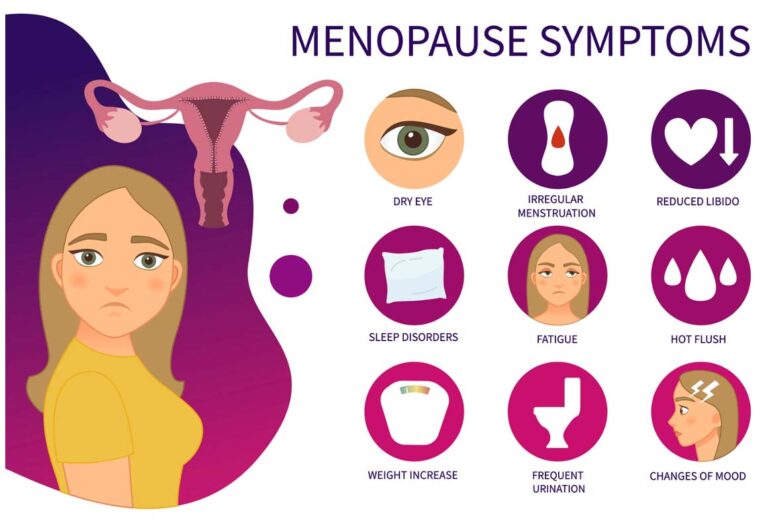
Symptoms an individual can experience during perimenopause and menopause are many. The symptoms can vary widely from person to person.
It can be difficult for an individual with CF, and possibly more so for those individuals post-transplant, to identify potential causes of the symptoms, as there is often a crossover with symptoms related to perimenopause and menopause, to complications associated with CF and post-transplant.
Talking to your GP, and your CF care team openly about your symptoms can start the process of understanding the symptoms and the causes. Use of symptom scores such as the modified greene scale can assist in you being able to record the impact of symptoms and facilitate the conversation with your healthcare providers. It may be the specific cause is not able to be identified as only hormonal, or only CF, but working together with your healthcare providers will assist in helping you manage the symptoms and improve your quality of life.
Symptoms that may be more specifically relevant for physiotherapy implications are:
- Reduced bone mineral density
- Changes in lung health, these may include increased inflammation and infection
- Urinary stress incontinence
- Dry vagina and recurrent urinary tract infections
- Brain fog and difficulty concentrating
Talk to your physiotherapist and discuss options for further support and monitoring in the following areas:
- Exercise prescription to promote bone health (weight bearing and resistance activities)
- Close monitoring and support of lung health.
- Pelvic floor exercises/Bladder health education, referral to women’s health if necessary
- Bladder health education/referral to specialist GP for prescription creams.
- Support with strategies to maintain adherence with exercise and lung health regimens as these may be harder to sustain with changes in mental well-being and concentration.
- Support with healthy choices and building individual resources to manage symptoms, including mindfulness, meditation, cooling cushions, hand-held fans for example.
Management of perimenopause and menopause is focused on improving symptoms, adjusting and accepting some of the changes, preventing and maintaining bone/lung and pelvic health, and improving quality of life. It is a time of change that will occur, but with support and appropriate management can be managed.