MENU
Autogenic Drainage
Please speak to a physiotherapist or your CF medical team before commencing any new treatment. DO NOT start using a device, or technique, on this website if you have not discussed this with your CF team first.
Autogenic Drainage (AD) is a technique that uses controlled breathing (changing your breath in and out – inspiratory and expiratory airflow) at different lung volumes to help loosen, mobilise and clear secretions whilst aiming to avoid airway closure and wheezing. It was created by Jean Chevaillier in Belgium in 1967. AD can be performed independently, however it can take more time to learn as it requires listening to the “feedback” from your lungs eg. sounds such as crackles and wheeze, and feeling where the secretions are. It may be a little harder to master autogenic drainage so regularly check in with your physiotherapist who will be able to review your technique and together you can continue to develop your skills with this technique.
Components
- The cycle generally starts by breathing down to quite low lung volumes (ie. breathing most of the way out), and gradually increasing the volume and speed of the breathing in order to move secretions from airways deep in the lungs through to large airways closer to the mouth.
- Previously, the levels of breathing in AD have been described in 3 stages:
- Unstick
- Collect
- Evacuate
- More recently, AD has been described in a less structured way with focus on where the secretions are as opposed to three stages
- AD can be combined with a PEP or OscPEP device.
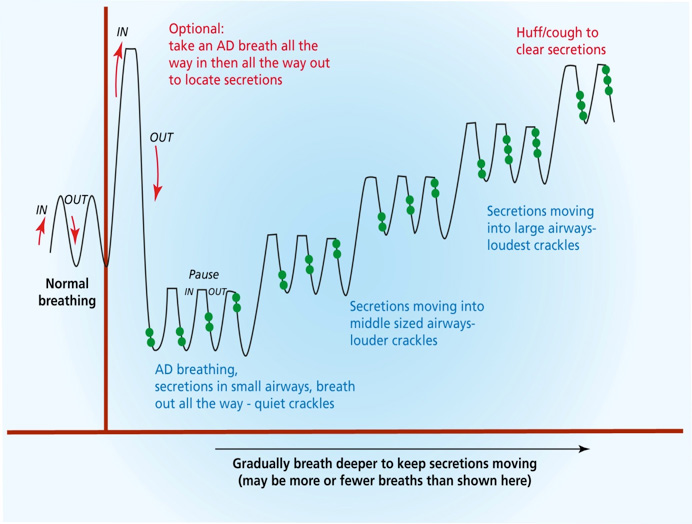
The diagram below is a schematic presentation of breathing during autogenic drainage. This is a guide only, the actual technique for you may vary and may differ to some degree from day to day depending on where secretions are moving or located.
The black line represents an example of autogenic draining breath depths, rhythm and volume. The highest point in black being the full breath in and the lowest point being a full breath out. The green dots represent the sound of crackles, indicating movement of mucus in the airways. You will see below that as the crackles are heard earlier in your breath out this suggests you should then change your breath volume.
Aims of AD
- To achieve the highest possible flow rate in each section of the airways to clear sputum towards the larger airways
- Breathing out in a controlled way so that the airways remain stable.
AD technique
- Seek assistance from an experienced physiotherapist when performing AD for the first time. AD usually requires multiple sessions of practice to learn the technique well.
- Whilst there are principles of AD that are important to learn, this technique is performed differently in different people depending on their symptoms on any given day
- Perform after or with your usual inhalation therapy (eg. Hypertonic saline, Bronchitol® )
- Use a position that seems most effective. Pay attention to your posture and positioning to avoid postures which may provoke gastro-oesophageal reflux (e.g. slumped sitting),
- The first inspiration can be a deep breath in with a pause at the top of the breath, before breathing most of the way out
- Initial breaths should be taken in through the nose using diaphragmatic (belly) breathing, each with a pause of 2-4 seconds, followed by breathing out actively using the abdominal muscles to empty the lungs
- Each breath out should be active but not too forced, aiming to increase airflow without causing airway closure (indicated by wheeze)
- Placing one hand on the abdomen and one on the upper chest can provide some feedback regarding the degree of expiratory force required and can help localise where the sputum is located.
- It is then important to adapt the breathing level and force depending on the “feedback” perceived such as the sensation of vibration of secretions and airway sounds
- Audible catching or crackling sounds at the end of the breath out are thought to indicate secretions moving from the small airways.
- When these sounds are heard earlier in the breath out, this indicates the need to increase the volume and speed of breathing whilst maintaining the same basic technique
- If feeling breathless, a larger breath in within normal breathing range can be performed whenever necessary before breathing out again towards lower lung volume
- Coughing should be avoided until mucus is felt in the large airways where it can be cleared with a high-volume huff or effective cough.
Other Practical tips when performing AD
- It is possible to breathe out via the nose but some auditory feedback may be lost compared to breathing out through an open mouth. Using a cylindrical mouthpiece or tube can assist during AD training.
- Some auditory feedback may be lost if combining AD with a PEP or flutter
Assisted Autogenic Drainage (AAD)
AD can be adapted for use in infants and young children, those unable to actively participate and those with severe exacerbation or advanced disease who cannot clear adequately without assistance. Specific training from a skilled physiotherapist is required to perform this technique.
In younger children AAD can also include gentle rhythmic bouncing on a therapy ball in well supported sitting to promote relaxation and enable effective AAD.