MENU
Principles of Airway Clearance
Airway structure
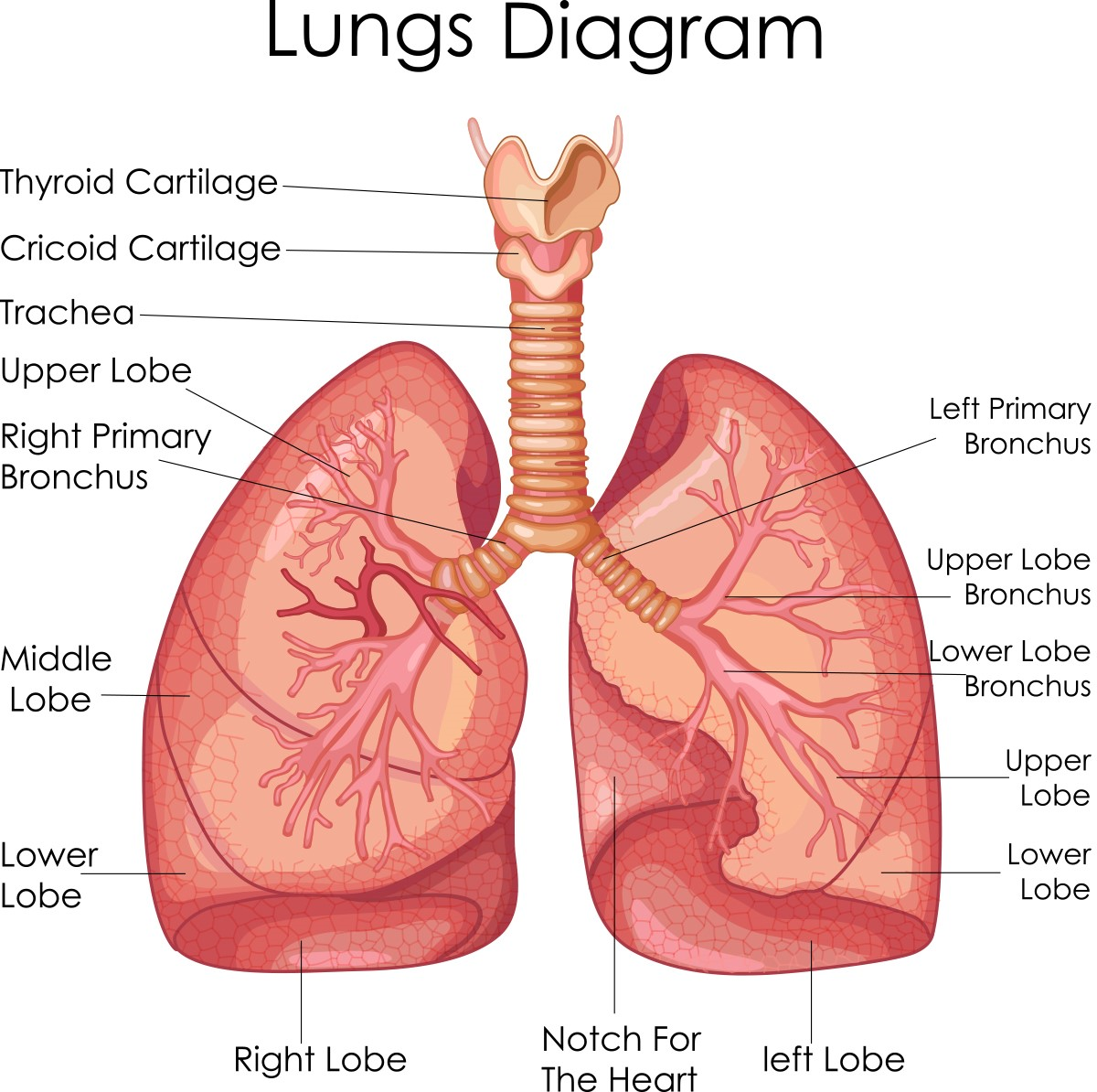
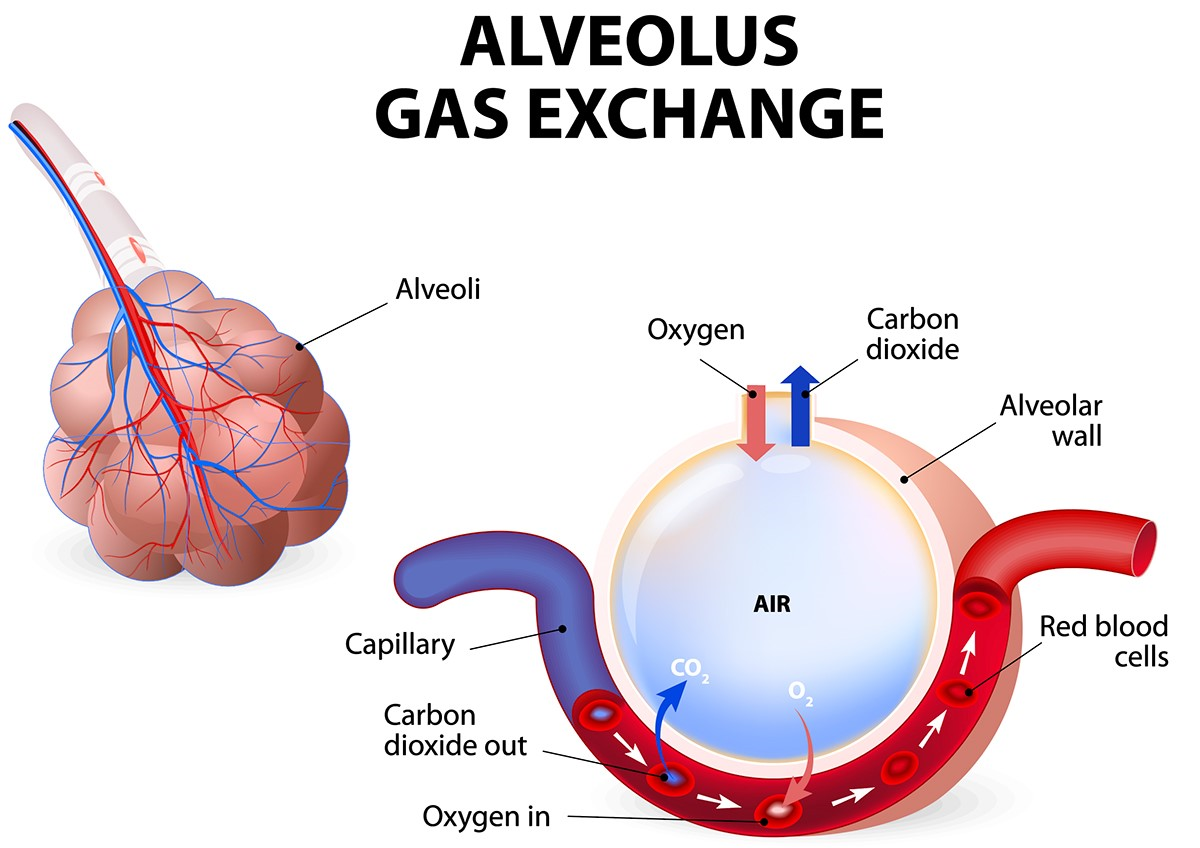
You can think of your airways like a tree that is upside-down. The trunk of the tree is your trachea (or windpipe) which then divides into your right main bronchus, which branches off into the airways of the right lung and the left main bronchus, which branches off into the airways of the left lung. The airways continue to branch off, getting smaller and smaller until they reach the alveoli (or air sacs) that fill up with air and allow the transfer of oxygen to the blood stream.
Airway obstruction
In the lungs, because the airway surface liquid layer is dehydrated, there is less of it, there can be a build up of mucus in the airways, it can’t move as easily, and bacteria from the air can get caught. This can cause inflammation (swelling) and tightness in the airways. As a result, air cannot move through the lungs as freely. Air movement is very important to help remove mucus from the lungs; with less air movement you can get more build-up of mucus which can lead to repeated infection which causes even more inflammation and airway damage over time. It is a vicious cycle.
Airway clearance helps to move the mucus up the airways towards the mouth where it can be cleared out of the lungs. Airway clearance can still be very effective in keeping your airways healthy even if you don’t produce a large volume of mucus when performing the techniques. Think of airway clearance like cleaning your teeth. When you clean your teeth every morning and night you don’t see large pieces of plaque fall into the sink. If you didn’t regularly clean your teeth then when you go to the dentist they may have to remove large pieces of plaque build up and your teeth may have been damaged permanently from the bacteria in this plaque. The same may occur in your airways, you need to regularly brush (or move air through all the little corners, crevices and airways) to stop the bacteria from creating an infection and causing damage to your lungs.
It is good if you can learn to become comfortable coughing out mucus so it can be tested for what bugs (bacteria) are growing. This helps doctors choose the best treatments for you, and will also help to keep you, and your team, informed for infection control reasons. Your mucus, or sputum as some people may call it, can also be used to monitor your lung health. The colour, texture or thickness and amount of your mucus, may help you understand what may be happening in your airways.
Understanding air movement in your airways
Coughing
When we cough our abdominal (tummy) muscles tighten and we close off our glottis (or throat) to create pressure in our lungs. Releasing this air then causes a forceful movement of the air outwards, a cough. This can move any secretions in the larger airways, the trachea and bronchi. Excessive coughing is tiring and can put a lot of pressure on the airways and over time may cause the airways to become floppy and damaged. A cough will not effectively clear the mucus from the smaller airways, so it is important you learn airway clearance techniques that will help move the mucus up to the larger airways so it can be cleared with the least amount of coughing.
Airway clearance techniques can help by:
- changing the way the air comes into the lungs
- changing the way the air comes out of the lungs
Changing the way the air comes in
To move mucus sitting in the airways the first thing you need is air behind it. There are many techniques to help get air behind the mucus. Some simple techniques are listed below:
- Taking a slow, deep breath. By breathing in slowly and purposefully, there is more time for air to make its way behind mucus.
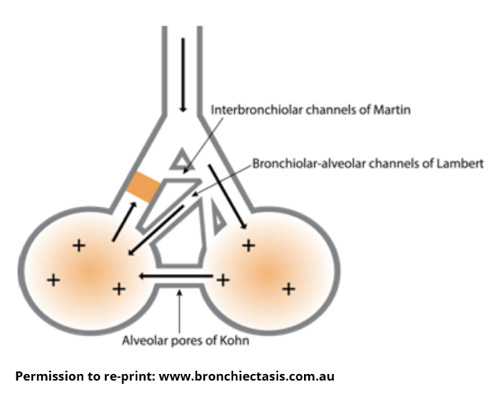
- Holding your breath for a few seconds once you have inhaled (breathed in) fully. The small alveoli (air sacs) in the lungs are connected to neighbouring alveoli by little bridges or channels. Holding your breath for 2-3 seconds allows air to travel through these connecting channels so it can find its way behind trapped mucus.
- Breathing out against a resistance (eg. Positive expiratory pressure, PEP). When you breathe against a resistance you create a pressure back into your lungs towards your airways which helps to splint (hold) the airways open. With repeated breaths against a small amount of resistance the volume in the lungs is temporarily increased which means there is more air behind mucus. PEP devices include a resistor and are used to create this effect. The amount of resistance and pressure need to be reviewed and set by a physiotherapist. Be aware that more resistance is not necessarily better!
Changing the way the air goes out
To move mucus there needs to be enough airflow (movement of air) over the mucus to unstick it from off the walls of the airways and up towards the mouth. Care must be taken not to force the air out too hard as this can cause the airway to narrow and sometimes close. It can also cause early or uncontrolled coughing which doesn’t help with clearance of mucus from the smaller airways. Some techniques to assist with airflow out of the lungs include huffing (forced expiration techniques). You can learn more about this in the Forced Expiration Technique section .